Gene Manipulations for Hemoglobinopathies
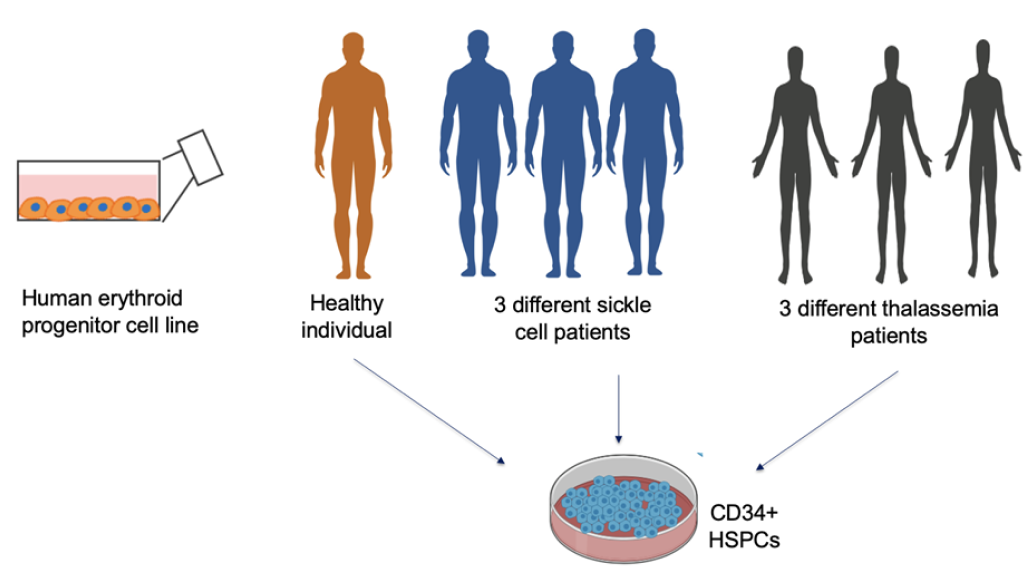
Transfusion-dependent Thalassemia and Sickle Cell Disease are two of the most prevalent red cell disorders, affecting millions worldwide. These genetic conditions often result in severe complications, including chronic anemia, progressive organ damage, a poor quality of life, and significantly reduced life expectancy. While traditional treatments like packed red cell transfusions and iron chelation therapy offer temporary relief, they fail to provide a long-term solution.
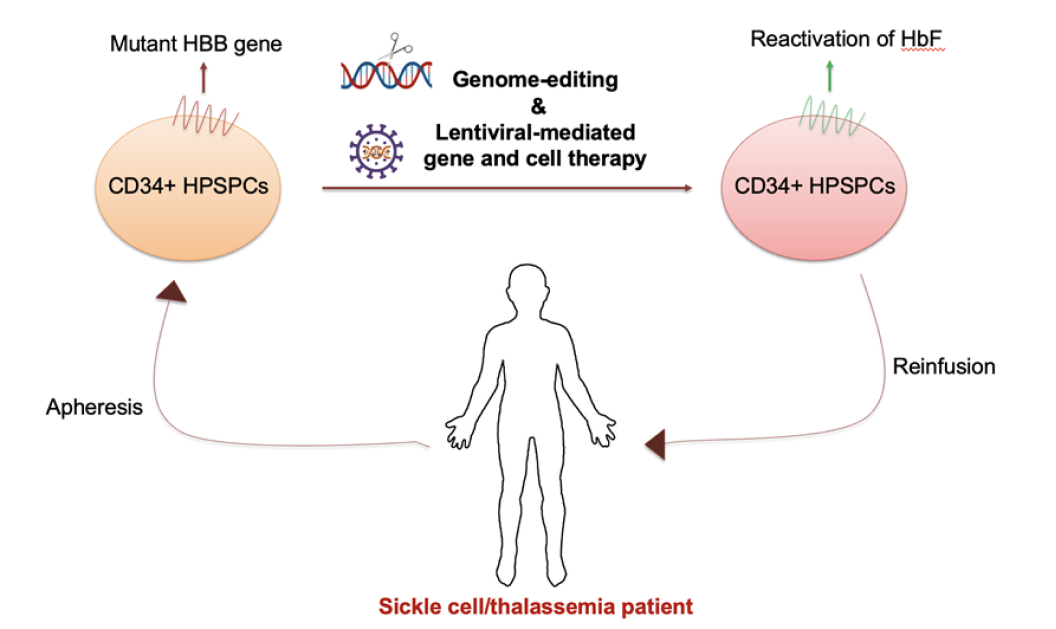
Hematopoietic stem cell transplant has come a long way but still faces inherent challenges, such as the need for high-dose chemotherapy, serotherapy, and allogeneic donors, which increases the risks of graft failure and graft-versus-host disease as the HLA barrier widens. Additionally, long-term immune suppression heightens the risk of severe infections, making this method less ideal. In contrast, innovative approaches like autologous gene-corrected transplants are emerging as safer and more effective solutions, with reduced reliance on immune suppression and improved long-term outcomes.